Academics
Overview
The program aims are to graduate residents capable of independent practice and ready for deployed medicine, to provide background in all orthopedic disciplines, and to promote advocacy, research and self-directed, adult learning.
Our goals created to reach the program aims are as follows:
• Facilitate a balanced education that fits within the framework of the ACGME core competencies
• Resident completion of sufficient case numbers for competency and confidence
• Support an academic program that provides a foundation for adult learning
• Foster a solid research foundation that furthers a spirit of investigation
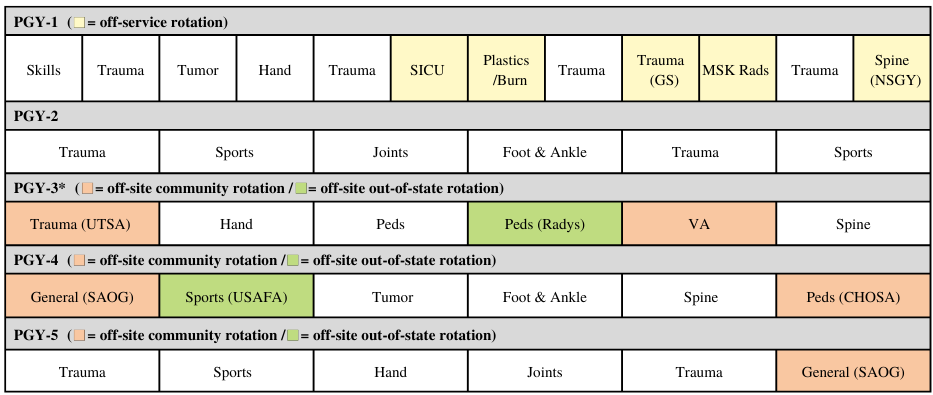
Clinical Rotations Sample Matrix
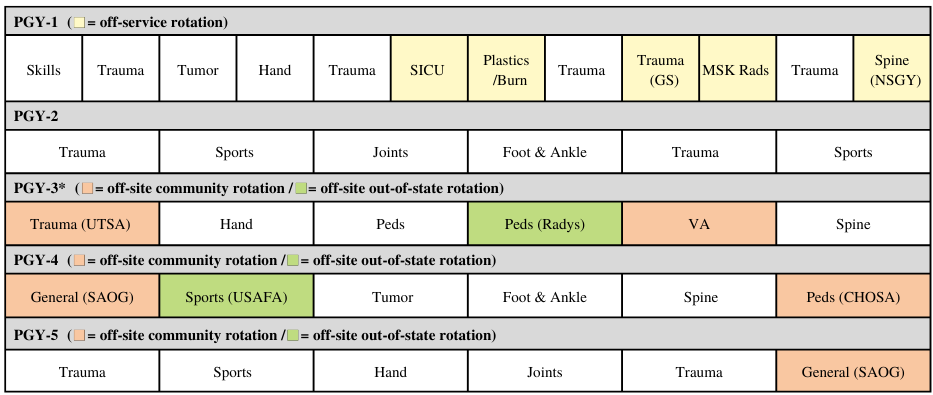
Post-Graduate Year Breakdown
PGY I
All of intern year is completed in San Antonio. Six months are dedicated to orthopaedics during which interns will work on trauma, tumor and hand services. They will get early experience taking consults and trauma call, reducing fractures and trauma management. The remaining six months are dedicated to non-orthopaedic rotations. Interns rotate through trauma surgery, plastic surgery/burn service, neurosurgery, basic surgical skills, surgical intensive care unit (ICU), and musculoskeletal (MSK) radiology.
Conferences/Training Courses: "Intern boot camp" (combination of lectures, cadaver and sawbones-based labs), ATLS offered to those interns attending the Combat Casualty Care Course.
PGY II
Second year residents remain in San Antonio and have increased responsibility with in-house primary call and intern supervision. From this point forward all rotations are orthopaedic disciplines. Second year residents rotate through trauma, foot and ankle, sports, and adult reconstruction. They work directly with and are supervised by the chief residents and staff and take an active role in teaching and supervising the interns.
Conferences/Training Courses: AO or OTA Basic Fracture Course
PGY III
Third year of residency is comprised of orthopaedic rotations at SAMMC (hand, pediatrics and spine services), University Hospital in San Antonio, Rady Children's Hospital in San Diego, CA, and the San Antonio VA Health System. Third years take trauma call and pediatric call during the course of outside rotations. They earn more independence as more operative experience is gained.
Conferences/Training Courses: AAOS/AHKS Resident Arthroplasty Course
PGY IV
Fourth year marks the beginning of senior-level responsibility, including home call instead of in-house. Residents rotate at SAMMC through spine, foot and ankle, and tumor services. They complete away rotations at the United States Air Force Academy in Colorado Springs, CO. They also work with the San Antonio Orthopaedic Group (SAOG) for adult reconstruction and sports and at The Children's Hospital of San Antonio (CHOSA) for a pediatric rotation. Residents gain more autonomy in the operating room and get to participate in a variety of experiences at different facilities which broadens their surgical experience.
Conferences/Training Courses: Enneking Seminars in Musculoskeletal Pathology.
PGY V (CHIEF YEAR)
Chief residents remain in San Antonio for the entire year. During this final year of general training, residents finalize their skills in operative specialties pertinent to generalists in any military practice. They are also charged with the education of junior residents. Depending on their schedules, chief residents rotate through trauma, sports, adult reconstruction and hand services. Chief Residents have day and night call responsibilities supervising the junior residents and the operating room.
Conferences/Training Courses: Three elective courses are offered based on the chief residents’ needs/desires. Each PGY5 will attend one of the following courses:
• Arthroscopy Association of North America & Society of Military Orthopaedic Surgeons Shoulder Arthroscopy Course
• AO Advanced Principles of Fracture Management Course (gives additional focus on management of more complex periarticular, pelvic and acetabular fractures)
• International Congress for Joint Reconstruction Hip & Knee Course (includes small group didactics and cadaver labs with a renowned international faculty)
Didactic Schedule
Didactics occur weekly on Wednesdays from 0700-1100. The curriculum focuses on essential topics in orthopaedics. Faculty surgeons provide expertise during core-topic lectures whiles residents facilitate discussion with case-based presentations and peer-to-peer instruction. Quarterly Visiting Professors provide in-depth knowledge and experience over a two-day visit. Journal club is conducted monthly. The program incorporates simulation and sawbones/cadaver labs regularly. Common components of didactics include:
• Built-in team training with team specific curriculum
• Peer-to-peer teaching
• Surgical indications conference
• M&M conference monthly
• Surgical simulation Labs
• Surgical cadaveric skill sessions
• Comprehensive Competency-Based Education--direct observation of surgical and clinic performance with extensive structured feedback. Innovative quantitative determination of resident skills pioneering education beyond ACGME and ABOS requirements.
Journal Club Structure
Journal club typically occurs once a on a rotating basis of subspecialties. Dinner is sponsored by industry and will typically include structured discussion of 3-4 articles of a specific subspecialty.
Visiting Professors (2021-22 Academic Year)
• Antonia Chen, MD, MBA – Brigham & Women’s Hospital, Adult Reconstruction, Director of Arthroplasty Research
• Jack Flynn, MD – Children’s Hospital of Philadelphia, Chief of the Division of Orthopaedics
• John Kelly, MD – University of Pennsylvania, Director Shoulder Surgery
• Min Kocher, MD, MPH – Boston Children’s Hospital, Chief of the Division of Sports Medicine
• Steven Parada, MD – Augusta University, Director of Shoulder Surgery
Clinical Sites
SAN ANTONIO MILITARY MEDICAL CENTER
SAMMC is our main clinical site and the only level one trauma center in the Department of Defense.
• The primary training site for all orthopaedic subspecialties
• 31 first-start cases per week in the operating room
• 4,500 cases annually with over 1,000 orthopaedic trauma cases including 1600+ individual trauma procedures
• 425-bed facility with expansion capabilities to 613 beds
• 32 operating rooms
WILFORD HALL AMBULATORY SURGERY CENTER
WHASC offers a new state of the art ambulatory surgery center and outpatient clinic.
• Outpatient clinic and surgery center for hand, foot & ankle and sports subspecialty services
• 7+ orthopaedic first-starts per week in the operating room
• 750 cases annually
• 4 operating rooms
UNIVERSITY OF TEXAS HOSPITAL
The other Level 1 Trauma Center in San Antonio which hosts our PGY3 residents. Each resident logs an average of 120 primary cases during the rotation.
THE SAN ANTONIO ORTHOPAEDIC GROUP
PGY4 site for adult reconstruction/general orthopaedics in a high-volume private setting. Residents participate in 400 cases each year.
AUDIE L. MURPHY MEMORIAL VA HOSPITAL
Adjacent to University Hospital, this is the site of the PGY3 general orthopaedics rotation with significant autonomy and exposure to pathology. Residents perform over 300 cases each year.
CHILDREN’S HOSPITAL OF SAN ANTONIO
SAMMC has developed a renewed partnership with San Antonio’s premier Children’s Hospital. Under the leadership of Dr. Elizabeth Magnabosco, rotating residents develop their growing pediatric surgery skills in a local setting. Residents performed over 500 cases at CHOSA per year.
RADY CHILDREN’S HOSPITAL SAN DIEGO
One of the premier children’s hospitals in the world, SAMMC enjoys a long relationship with Rady’s where residents get a broad experience in pediatric trauma, neuromuscular disorders, deformity correction and other pediatric complaints. Residents average over 130 primary cases during their two-month rotations.
UNITED STATES AIR FORCE ACADEMY HOSPITAL
This is the location of a sports-based rotation for PGY4 residents, including experience as a team physician for NCAA Division 1 teams. Residents average approximately 100 primary cases each rotation.
Call Requirements
PGY-2 residents are responsible for in-house overnight call at BAMC. With a class of 6 residents, this occurs on a rotating basis throughout the week, typically averaging to be 1-2 nights of primary call thought out the week depending on the rotation.
Chief call is spread out among the PGY-4 and PGY-5 classes on a rotating basis and taken from home overnight and on the weekends. Chief call over the weekends and holidays are typically spent in the operating room covering trauma cases with co-residents.
Mentorship Program
We currently have staff representing all subspecialties with various professional, academic and leadership roles in the department, who are all eager to serve as mentors for residents. Mentors are not assigned to residents, but instead residents are encouraged to seek out faculty with shared interests and career goals to facilities the best use of a mentor-mentee relationship.
Opportunity for Meeting Attendance
Every year residents are sponsored to attend the SOMOS annual meeting to present their research abstracts. There are additional funding opportunities for residents to attend and present their work at multiple subspecialty conferences at the local, regional and national level.
Does the program provide Loupes/Lead?
Loupes and lead are currently provided and paid for by the department.
Does the program provide any textbook funding?
There is no textbook funding from the department. However, there is a yearly bonus that increases across each training level for active duty residents that could be used for textbooks as needed.
|