Academics
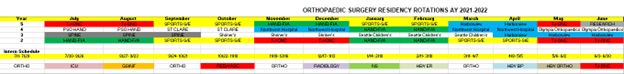
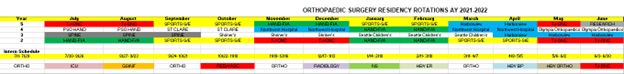
The structure of the Orthopaedic Surgery Residency curriculum is currently as follows:
R1 year: Rotations consist of six 4-week rotations of Orthopaedics (Madigan, Harborview) and seven other intern rotations (Neurosurgery, Vascular Surgery, General Surgery Night Float, ICU, Harborview ER, Harborview Burn Center, and Musculoskeletal Radiology).
R2 year: Rotations consist of six 2-month rotations at Madigan, with an emphasis on developing a strong foundation of Orthopaedic knowledge and surgical skills across the major orthopaedic sub-specialties: Sports Medicine, Shoulder-Elbow, Hand, Foot-Ankle, Adult Reconstruction, and Musculoskeletal Oncology.
R3 year: Rotations consist of four 3-month rotations in: Orthopaedic Trauma at Harborview, Pediatric Orthopaedics at Seattle Children’s Hospital, Pediatric Orthopaedics at Shriners Hospital for Children, and Adult/Pediatric Spine Surgery at Madigan.
R4 year: Rotations consist of 2-month rotations in: Adult Reconstruction at UW-Northwest Hospital, Hand and General Ortho at Puget Sound Orthopaedics, Foot-Ankle at Olympia Orthopaedic Associates; Hand and Foot-Ankle at Madigan.
R5 year: Rotations consist of five 2-month rotations at Madigan in the major orthopaedic subspecialties, 2-months as Orthopaedic Trauma Chief Resident at Harborview, and additional time for research and board preparation.
Sample Matrix
Didactic Schedule including opportunity for labs/simulations
Conferences are held on a regular basis. Morning report is held daily at 0645 after morning rounds. All of the previous night’s (or weekend’s) cases are presented. This is followed by specialty lectures Mondays and Tuesdays, OITE quizzbowls Wednesdays, and Trauma post-ops Thursdays. Friday is academic day. Residents, staff, visiting staff, other medical staff, and administrative personnel may present lectures. In addition there is monthly Journal Club, QA and Morbidity and Mortality conferences on alternating months.
The Orthopaedic Research Director conducts the orthopaedic research conference quarterly. At this conference updates on ongoing research projects are presented, difficulties encountered in research projects are discussed and new ideas are examined. In addition, announcements are made regarding possible presentation forums for research projects and regarding resident research paper competitions.
Our quality assurance/quality improvement conference (QA/QI) is held monthly. During this conference all morbidities and mortalities from the previous month are reviewed. Residents and staff present cases, which are then thoroughly discussed. Where appropriate, issues for ongoing review are identified or areas in which process or technical changes could be expected to benefit patients are explored. This conference provides another opportunity to discuss both medical/ethical and risk management issues.
In the first quarter of the year we schedule Friday morning conferences for intensive anatomy course. We obtain a cadaver for prosection each year. The sessions begin with a cadaver prosection presented by the junior resident who has performed the prosection supervised by the staff. Orthopaedic teaching staff participates in these lectures as appropriate to their area of subspecialty expertise. Following the prosection, the designated staff presents a formal lecture regarding that anatomic area. In this manner over a period of several months, the musculoskeletal system is completely dissected and reviewed.
Journal Club Structure
This year we are revamping journal club and hosting it at locations outside of the hospital. We meet at either an attending’s house or at a restaurant and discuss articles in a more relaxed setting. Juniors are assigned to an article with a senior assigned as well to help comment on articles and generate discussion with staff who bring their own knowledge and expertise on the matter. Recent articles from multiple orthopaedic journals are selected for review. We discuss not only the clinical aspects of journal articles but also the research design and validity of the conclusions drawn based on the power of the research.
Clinical Sites
The Madigan Orthopaedic Program has five participating Institutions:
1) Harborview Medical Center in Seattle, Washington: Harborview is a nationally recognized institution specializing in the treatment of trauma. Residents rotate there three times during their residency. First, during their PGY-1 year, they rotate for a month each in Emergency Medicine, Orthopaedics Night Float, and Burn Surgery learning to care for multi-trauma patients. Second, during their PGY-3 year, they rotate for three months as part of an orthopaedic trauma team where they receive both operative and non-operative training in multi-trauma patient care. As juniors on the trauma team, they take primary trauma call at an average of q3-q4 call. Finally, in their PGY-5 year for two months, they are Chief Resident of a trauma team. They assume major surgical responsibility for the care of trauma victims, supervise, and instruct junior trauma team members on inpatient care of patients.
2) Shriner’s Hospital for Children in Spokane, Washington: Residents rotate for three months during their PGY-3 with different orthopaedic staff. The Shriner’s is primarily a tertiary referral center that cares for an exclusively pediatric population with complex orthopaedic conditions including cerebral palsy, myelomeningocele, scoliosis, and congenital and other acquired orthopaedic conditions. The Shriner’s program is exceptionally strong academically with multiple conferences and journal clubs per month, a gait lab, and excellent opportunities for research.
3) Seattle Children’s Hospital, Seattle, Washington: The Seattle Children’s Hospital staff includes a number of nationally recognized pediatric orthopedists. Residents at Children’s are exposed to a broad spectrum of elective pediatric reconstructive surgery and pediatric trauma. They also participate in a number of multispecialty clinics dealing with a broad range of complicated pediatric orthopaedic conditions. This is a three-month rotation during their PGY-3 year.
4) Puget Sound Orthopaedics and Lakewood Surgery Center/ St. Clare Hospital, Lakewood, Washington: Puget Sound Orthopaedics is one of the largest private orthopaedic practices in the area and serves the Puget Sound region with comprehensive orthopaedic care in musculoskeletal disorders. The team comprises nine board certified surgeons with sub-specialties ranging from shoulder, upper and lower extremity, and sports medicine to spinal and podiatric care. Residents rotate for three months during their PGY-4 year in adult reconstruction and on the hand surgery service. The rotation has both operative and clinical experiences. The residents work closely with the attending staff on a one on one basis, and play an integral role in the function of the team.
5) Olympia Orthopaedic Associates/ Providence St. Peter Hospital, Olympia, Washington: PGY-4 residents rotate with a Foot and Ankle Surgeon at Olympia Orthopaedic Associates where they receive a diverse and well-rounded educational experience in Foot and Ankle Surgery for the residents to supplement their training at Madigan. This is a two-month rotation during their PGY-4 year.
6) Northwest Hospital, in Seattle, Washington: PGY-4 residents spend two separate two-month rotations at Northwest Hospital, which is the premiere Adult Reconstruction hospital in the Pacific Northwest. There they work with University of Washington staff surgeons who perform both complex revision arthroplasty as well as high-volume primary arthroplasty.
Call Requirements
Call is taken from home and averages every third to fourth night. Orthopaedic PA residents, PGY-2s, and the PGY-3 on Spine at Madigan take junior call. Madigan is a Level 2 Trauma Center. Residents are required to perform the initial evaluation of patients with musculoskeletal trauma in the Emergency Department as well as the initial evaluation for in-house urgent consultations.
PGY-4 and PGY-5residents pull senior call. They provide back up for the primary call resident and take responsibility for the evaluation, treatment and appropriate disposition of patients seen in the Emergency Room or in-house consultations. They are responsible to inform and consult with the staff on call as appropriate. Staff is always immediately available.
Mentorship Program
Madigan was previously a mentorship model, but has recently switched to a team-based model. Given our low resident-to-faculty ratio, elements of the mentorship model remain ingrained in our program. Often residents are one-on-one with staff in clinic and in the operating room. We also benefit from the team model with senior resident oversight for junior residents assigned to their team. Staff surgeons are heavily invested in resident mentoring and development.
Opportunity for Meeting Attendance
Yes, residents are able to make it to multiple meetings per year.
Does the program provide Loupes/Lead?
Yes, the program pays for both Loupes and custom lead
Does the program provide any textbook funding?
No
|